Providing Accessible Patient Education
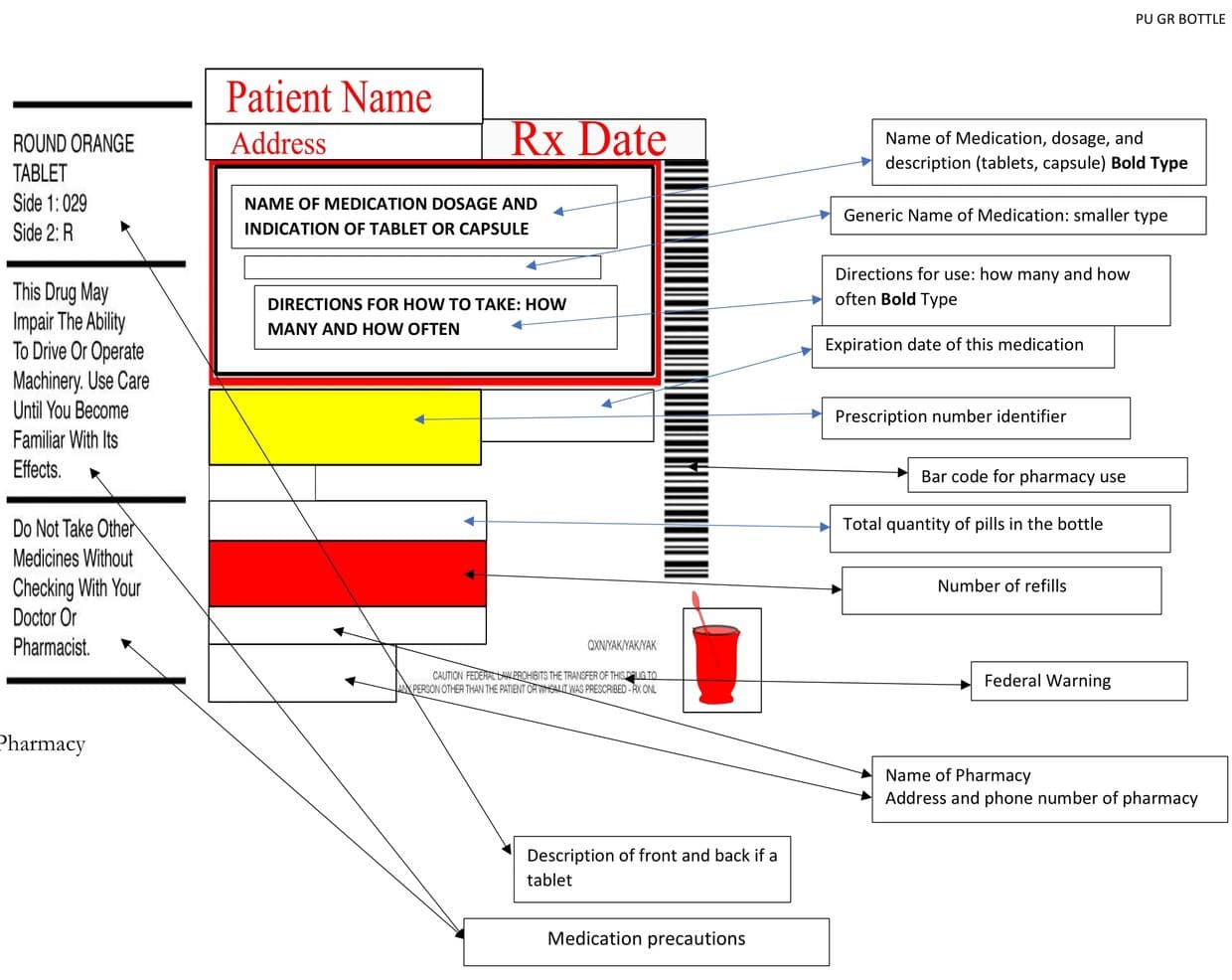
Medication Label
Medication Label Reference Graphic
Use the Medication Label graphic when reading the Medication Safety Sections for further information.
Find Out More: Hit button below to link to CDC website regarding Medication Safety Program
Healthcare Communication
MEDICATION SAFETY
Medication Label Overview
The above graphic is a “typical” label found on most medication bottles. The information may be arranged differently but contains the same information.
Why Is this Important? SAFETY
Great idea to get into the habit of checking you medication bottle when filling your prescription.
Is the Name Correct?
You would be surprised how many people have the same name. Your address can be used to further identify that this prescription is for you.
Expiration Date:
Some medications can degrade over time. Effective until expired, in other words. No telling what danger lurks when taking expired medication.
Medication Precautions:
Short description on bottle to tell you if you need to take with food or without food, and many more types of precautions. A more complete listing can be found on the print out from the pharmacy that came with your prescription. Be on the look out for any directions pertaining to crushing or cutting. Some medications should not be crushed. If you have trouble taking large tablets, discuss this with your prescribing professional at the time you are getting your prescription. If you forget, the pharmacy can call your healthcare provider, but this may cause a delay. Your pharmacist is a resource person anytime you have questions when filling your prescription. You should feel free to ask questions.

The Precaution
“Do not operate machinery while taking this medication” : Often times, people forget that a vehicle is a “machine”. If this precaution appears, probably a good idea not to drive when taking such medicine.
Directions for taking
Most likely, a medication bottle has either tablets or capsules. Liquid medication may not come in a bottle, but will have a similar label. This area will indicate how many tablets/capsules and how often. It will also indicate liquid dosing as well.
BE AWARE: SAFETY ALERT
When re-dispensing your tablets/capsules into a pill organizer, be careful to distribute them in your organizer according to how you are directed to take them. Use care anytime you are taking medication out of a bottle and placing it in a container other than the one it came in. Once a pill/capsule/any medication leaves its original container, you no longer have the luxury of the label. Labels are there for a reason and follow federal guidelines.
Number of refills
You may be surprised to learn that some people are concerned when they have no refills for some medications, like an antibiotic. Antibiotics are one type of medication that is prescribed for a certain period of time, then the prescription ends, no refills. For some medications, they are not intended to be taken for extended periods of time. Hopefully, this very subject was discussed when the medication was prescribed so that you won’t be surprised when you receive your medication.
Pharmacy
Name, address, and phone number. If you get home and something isn’t right, you’ll have the information for contacting the pharmacy right on the container the medication came in. If ever a question, don’t hesitate to call the pharmacy.
Federal Warning
The entire process of medication prescribing and distributing is highly regulated. This is for your safety. The warning is a reminder that your medication was prescribed to you and not anyone else. It’s a reminder not to share.
Saving Medications
Your prescription container has a date that it was filled. You might be surprised to learn that people will “save” certain medications for various reasons. There are all kinds of reasons not to “save” unless you have been specifically directed to do so by a licensed medical practitioner.
Not everyone is truly laser focused on their medications. So, visual pill identification is not necessarily done by a lot of people. However, if a medication is one that you are familiar with and have been taking, it’s not a bad idea to get familiar with what it looks like-shape, color, size, because you might find that it can be useful. For example, if you receive your prescription and your medication doesn’t look right, you’ll be alerted to do further checking.

Dosages
dosages are confusing to a fair number of people. Basically, it’s the strength of a particular medication. Medications with the same name can come in different “strengths”. This can be confusing in certain situations. In a hospital for example, you may be used to taking one tablet of a certain medication at home, but the hospital has given you two instead. This is the time to speak up. There really is no replacement for knowing your medications, especially those you take on a regular basis.
Bringing Your Medications With You to the Hospital
Many times, patients do not keep an up to date lisings of their medications, instead, they choose to bring their medicines with them to the hospital. If your medications are in labeled medicaiton bottles, they are easy for the hospital staff to read. (This is true for any healthcare facility).
If you bring a pill organizer without anything to identify the medication, this can be a lot tricker. It should be mentioned here, that when you are admitted to a hospital, you should not be actually taking your own medications from home unless specifically directed to do so. There are many reasons, but an obvious one is that the people treating you in a hospital will be unaware of what you are taking, which isn’t a good idea. To keep medications safe, have someone you trust to take the medications home for you so that they don’t get lost.
Pain Medication
This is such an important subject that it will be mentioned several places at the Patient University™ because of some particulars associated with pain medicine. The subject warrants specific education and attention, however, in this context, one area specifically will be mentioned. In a hospital, pain medication is one area of a lot of misunderstanding and miscommunication, resulting in a lot of patient/family frustration.
Pain Medication: The Process
A medication is ordered by a licensed healthcare practitioner, a physican, a nurse practitioner, or a physician’s assistant. Typically, nurses administer or “give” the medication to the patient. With pain medication, there are “parameters” or dosing guidelines. For example, for mild pain, “x” medication is orderd. For moderate pain, “x” is ordered, and so on. Sometimes, a pain medication is ordered to be given at a certain time, while most pain medications are ordered on a “prn” basis. This “prn” means as needed.
What this Means to a Patient
That pain medication, most likely will not be administered/given unless asked for by the patient. This is the source of a lot of confusion. A pain medication has limitations, meaning you can have a prn “as needed” medicine, but only a certain dose in a certain amount of time. It does not mean it will be given automatically or at a specific time. There are exceptions to this, but it is not the rule. For example, a pain medicine may be ordered “for moderate to severe pain every 6 hours prn/as needed”. This means that the pain medication can be given, but no sooner than every 6 hours. It also means that the patient will need to contact the nurse and let them know they are having pain/discomfort and that pain medication is being requested.
Important discussion
If there is pain that is not being relieved, patient/family need to speak up. When the patient sees the physician or any other licensed medical practitioner, be encouraged to discuss this issue with them so they can decide the best pain medication regimen. The patient/family should discuss this with the assigned nurse as well. Note, that when pain medication is requested, BEFORE the nurse is allowed to administer it-(TOO EARLY), more than likely the patient/family will have to contact the nurse to request the pain medication when it becomes available. The patient probably will not get the pain medication requested, if it was requested too early.
Some nurses will anticipate the need for pain medication within the time window, and will speak with the patient regarding the need for pain relief. This varies widely. Remember the time frame. If patient can have said pain medication every 6 hours, then know when it can be requested again. The process takes time. The first challenge is to notify the nurse-this can take time. The nurse will need to retrieve the medication-also takes time. If you request the pain medication too early, start the process over.

Be Aware
Common in a hospital setting is a request for pain medication. If the patient requests pain medication from someone other than the nurse, there will be a delay in getting that pain medication. The person the patient notifies of pain must contact the nurse, then the nurse will need to determine if it is within the time frame to be given, at the very least.
Communication in a hospital varies so widely, there is no one foolproof process. However, if you know that the nurse is the one that needs to administer the pain medication, then it may be helpful to know that this is the person to talk to directly, if at all possible. Given the atmosphere within hospitals, this alone can be a challenge. It will not hurt to tell a nurses’ aid you need pain medicine, however, remember the chain of communication is shorter if you can tell the nurse directly.
Pain Medication and the Pain Scale
The person administering pain medication will ask on a scale of 1-10 what pain level the patient is experiencing. (this scale if for patients that are able to answer) It is a scale used to determine the severity of pain so that the appropriate medication can be administered. It is also used after the pain medication is administered to evaluate the effectiveness pain relief.
Ideally, the person administering the pain medication will first ask what level of pain the patient is having. After it is administered, they should be following up with the patient to see how effective the medication was for the pain.
The goal is to find out if the pain medication lessened the pain. In other words, was it effective.
CHECK OUT THIS PAIN SCALE RESOURCE
One pain scale commonly used in hospitals is called the Wong-Baker FACES® Pain Rating Scale. You may be familiar with this scale. It is the scale of 1-10 for rating pain.
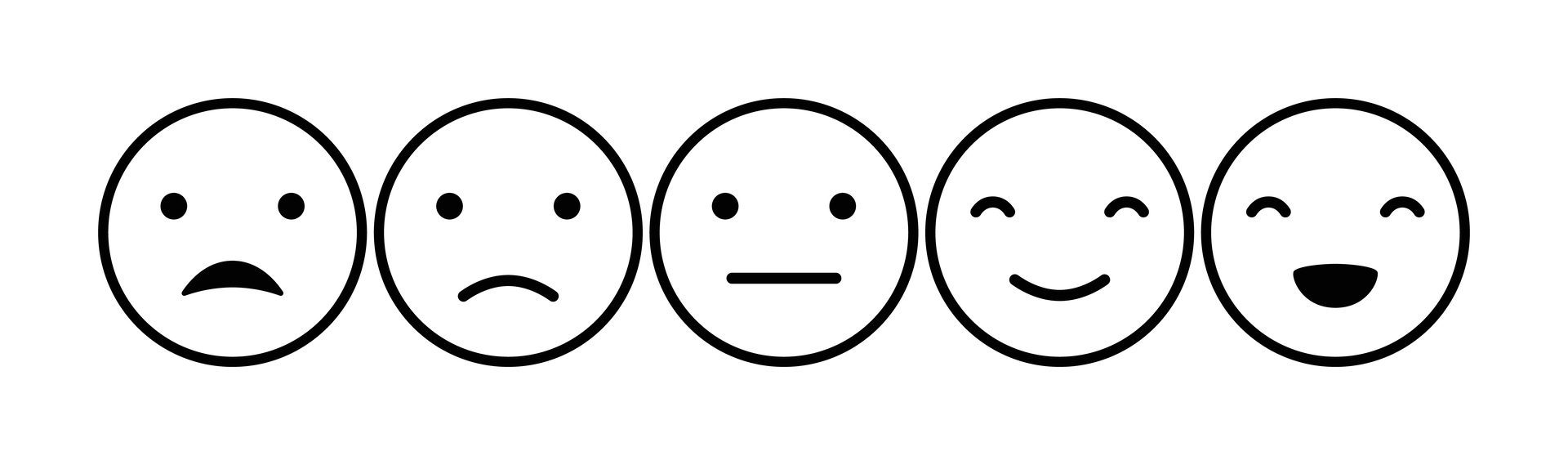
- 0-No Hurt
- 2- Hurts a little bit
- 4-Hurts a little more
- 6-Hurts even more
- 8-Hurts a whole lot
- 10-Hurts worst
Note that there are graphic depictions of faces along with this scale.
“This tool was originally created with children for children to help them communicate about their pain. Now the scale is used around the world with people ages 3 and older, facilitating communication and improving assessment so pain management can be addressed.”
Please know that this is not the only pain scale in use within a hospital. For example, in ICU a pain scale appropriate for unconscious patients is commonly used.
Reference: Bibliography
Citation: Wong-Baker FACES Foundation (2020). Wong-Baker FACES® Pain Rating Scale. Retrieved [Date] with permission from http://www.WongBakerFACES.org. Originally published in Whaley & Wong’s Nursing Care of Infants and Children. © Elsevier Inc.
Frequently Asked Patient Questions
The Patient University: One part of the “process” in the emergency room involves what is called “triage”. The basic explanation is the hospital and staff are determining who to treat first based on the how sick the patient is. They collect information to help determine and plan who they are treating and in what order. This process is slightly different in each hospital. Influencing factors may include but not limited to how many patients arrive at the emergency room at the same time, how sick are they, and many other factors.
SOLUTION: One of the best things patients/families/significant others can do to prepare for such an emergency is to have your up-to-date information handy. Naturally, we recommend the Patient Organizer so all your information is in one place. One very good reason for this is when you are ill, you won’t have to rely so heavily on your memory.
WHAT TO EXPECT: This section will be updated fairly often. If you have a particular question, you can email us your questions as well at thepatientuniveristy@gmail.com
Digital DownloadS
Download tip sheets, question reminders and more. Highly recommend placing them in your binder.
Videos
The Patient University Presents
With Your Host Pressure Injury Bob
Video Interviews And Podcasts
COMMUNICATION WITH YOUR HEALTHCARE PROVIDER
Does this sound familiar?
- No one told me…
- They never tell you anything...
- I told them; they just didn’t listen.
- No one told me it would take so long.
- They said I could go home.
- I have no idea what’s going on.
These are just a few very common statements by patients/families. Learning how to communicate with anyone in healthcare can be challenging.

Deep Dive
A basic definition of communication is an information exchange. In healthcare, communication can be tricky. One obvious consideration is the language of “healthcare”, in other words medical terminology. Healthcare professionals speak a different language to patients sometimes, and it can cause confusion. Add in some variables like being ill and not feeling well, and it can spell miscommunication.
Does this sound familiar?
A patient is expecting something, the healthcare professional is stating something, and the patient is left feeling their expectations were not met and questions not answered.
Scenario:
Healthcare professional is explaining something to the patient. Something is mentioned, the patient starts to think about whatever was said, the healthcare professional continues on explaining and doesn’t realize they left the patient behind. The patient doesn’t remember half the conversation because they were still at thinking about whatever it was when the healthcare professional continued on without the patient keeping up. It is exactly like learning Tai Chi you have to watch and practice hands, body movements, legs, and feet separately. You can’t watch all areas at same time, you have to learn them in a series. Same concept as communication with a healthcare provider.
With healthcare communication, there are no “traffic signs” which can lead to miscommunication.
Tips and Tricks for Better Healthcare Communication
Preparation:
Organize basic healthcare information and place in an organizer (Naturally, we recommend The Patient University’s My Patient Organizer)
- Basic Healthcare history:
- List any chronic diseases, allergies, past surgeries, list of physicians/medical offices, home health agency. Very helpful if you can include your primary care provider.
- List Any Treating Clinics:
- If you are being treated at an outpatient clinic or facility, include name and phone number.
- Demographic Sheet:
- This is information like who to contact in an emergency, home address, telephone numbers.
- Insurance information:
- Be sure phone numbers are working numbers. Provide alternate contacts and phone numbers as well.
- Medication List:
- List of current medications. Good idea to decide alphabetical or most recent. If you are really energetic about this, list them most recent and alphabetical order. Be sure to include any over the counter medication like vitamins, supplements, elixirs, over the counter pain medication and anything taken on a regular basis.
- If you use a pill organizer, you’ll still need this list, update as you go along.
- Tip Sheet for Asking Questions: (See our tips sheets)
- Reference the medication tip sheet anytime you anticipate a new medication. Read through the tip sheet. Recommend holding in your hand to remind you.
- Steno graph top flip journal:
- Spiral notebook
- Sharpie and pen and pencil paper clips and clips
- Calendar
- If at all possible, bring someone to all of your appointments. Four ears are always better than two!
Get to know the Processes
Learn the basic process of being a patient. Two general areas: In a hospital and out of a hospital.
Discharge From a Hospital
If you have a good idea how a discharge from a hospital works, you can prepare yourself and plan ahead. The goal here for understanding so that the patient/family can anticipate questions.
HOSPITAL DISCHARGE
- The hospital will plan your discharge from the moment you become admitted/official patient.
- Expect a case manager to visit you while you are in the hospital. They will ask you questions related to your home situation and any family caregivers and their involvement in your after care.
- Help determine if you can care for yourself at the place you were living prior to admission, and any special needs the patient may need after discharge.
To Be Continued…
Subscribe
Keep in touchUSEFUL WEBSITE LINKS
The Centers For Disease Control and Prevention “CDC”
National Institute of Health “NIH”
Centers for Medicare & Medicaid Services | CMS
U.S. Department of Health & Human Services
UOAA United Ostomy Association of America
Welcome to the Wong-Baker FACES Foundation (Pain Scale)
VA US Department of Veterans Affairs
AHRQ Agency For Healthcare Research and Quality
Patient Safety Organization (PSO) Program ( Advanced-regarding mishap reporting)
Department of Health and Human Services Office of Inspector General | Government Oversight
Department of Health and Human Services
Spotlight On… Adverse Events
AGENCIES Within HHS US Department of Health and Human Services
SAMHSA – Substance Abuse and Mental Health Services Administration
NIH National Institutes of Health
Indian Health Services The Federal Health Program for American Indians and Alaska Natives
HRSA Health Resources & Services Administration
FDA Food and Drug Administration
CMS Centers for Medicare and Medicaid Services
CDC Centers For Disease Control and Prevention
CDC Centers For Disease Control and Prevention Medication Safety
AHRQ Agency For Healthcare Research and Quality
Patient Safety and Quality Improvement Preventing Infections
ACL Administration For Community Living
Administration for Children and Families
USDA US Department of Agriculture